MRI Analysis Identifies Jaw Bone Defects Specific to MPS Types, Including Sanfilippo
Written by |
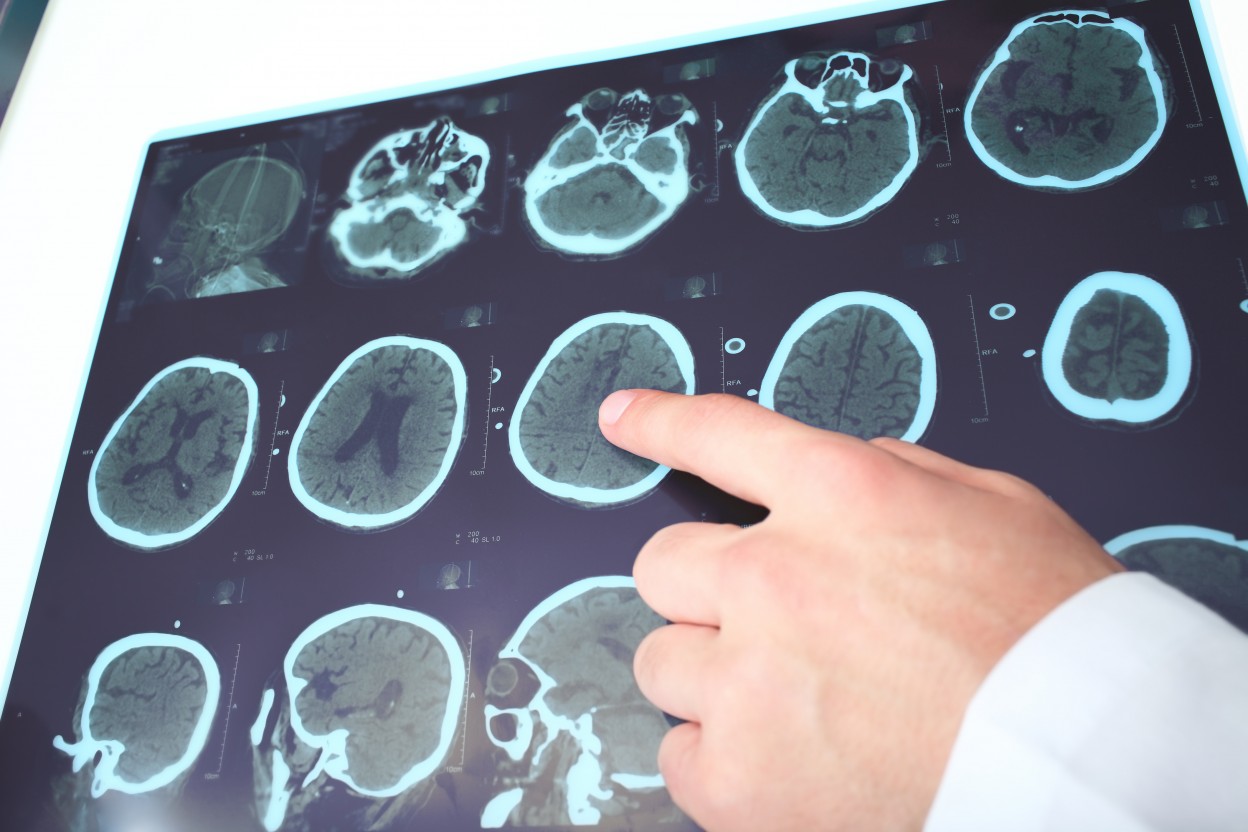
A retrospective analysis on magnetic resonance images from patients with mucopolysaccharidoses (MPS), including Sanfilippo syndrome, revealed jaw bone defects specific to certain disease subtypes.
Researchers also found that some of these craniofacial abnormalities, which are those relating to the bones of the skull and face, were not corrected even with successful stem cell transplants in patients with MPS I, also known as Hurler syndrome.
The study, “Differences in maxillomandibular morphology among patients with mucopolysaccharidoses I, II, III, IV and VI: a retrospective MRI study,” was published in Clinical Oral Investigation.
Craniofacial abnormalities are common features of almost all MPS types, and can affect chewing, speaking, and breathing, in addition to the social stigma patients may face.
For instance, a small upper or lower jaw bone is a risk factor for obstructive sleep apnea, a condition whose prevalence varies significantly among MPS types, with MPS I, II, and VI patients the most affected.
Despite these risk factors, no extensive imaging analyses have been done to characterize these abnormalities or test possible treatment effects until now.
In this study, a team of German researchers looked at magnetic resonance images (MRI) to analyze the morphology of MPS patients and evaluate the craniofacial effects of hematopoietic stem cell transplantation (HSCT) in MPS I patients, which is the treatment of choice for these patients.
HSCT is a blood stem cell transplant that uses stem cells derived from the bone marrow, peripheral blood, or umbilical cord blood. HSCT has been successfully performed in children with MPS I since 1980.
Its immediate benefits include a correction of enzyme deficiency and clearance of glycosaminoglycans (GAGs) which are sugar molecules that accumulate in MPS 1 patients, while long-term benefits include the possibility of long-term survival by protecting the heart, lungs, and brain from the effects of disease progression.
The study involved 27 healthy individuals used as controls, and 41 MPS patients with MPS I, II (Hunter), III (Sanfilippo), IVA (Morquio), or VI (Martoteaux-Lamy). All patients had been treated at the University Medical Center Hamburg-Eppendorf in Germany between 2009 and 2017.
No significant differences in upper jaw dimensions among patients with different MPS types were observed.
However, the dimensions of the lower jaw bone, or mandible, were smaller in MPS I patients than in MPS II and III patients as well as controls. This was found to be due to the degeneration of the lower jaw joint area (mandibular condyles), which is less severe in MPS II and absent in MPS III patients.
Importantly, these jaw anomalies — namely micrognathia, a condition where the the jaw is undersized — in MPS I patients were not improved with HSCT, and could therefore cause “esthetical and functional problems” even in successfully transplanted MPS I individuals.
According to the researchers, “clinicians should be aware of specific differences in mandibular morphology and condylar involvement among the MPS subtypes,” especially because of the serious effects it can have on patients’ breathing, which could be related to the “high prevalence of obstructive sleep apnea in MPS I patients.”