Sanfilippo Type A Causes Buildup of Sugar Molecules Besides Heparan Sulfate, Mouse Study Shows
Written by |
Sanfilippo syndrome type A leads to the accumulation of other large sugar molecules besides the characteristic heparan sulfate in several organs, according to a mouse study from Italy.
The study, “Glycosaminoglycan levels and structure in a mucopolysaccharidosis IIIA mice and the effect of a highly secreted sulfamidase engineered to cross the blood-brain barrier,” was published in the journal Metabolic Brain Disease.
Sanfilippo syndrome type A, also called mucopolysaccharidosis type IIIA (MPS IIIA), is caused by a deficiency in the enzyme heparan N-sulfatase, which is responsible for the breakdown of heparan sulfate — a specific type of large sugar molecule called glycosaminoglycans (GAGs).
This leads to the toxic accumulation of heparan sulfate within cells and tissues, causing cellular damage in multiple organs.
MPS IIIA mainly affects the central nervous system (the brain and spinal cord), leading to progressive neurodegeneration, with subsequent mental decline and behavioral disturbances.
Current enzyme replacement therapy (ERT) is ineffective at treating brain damage, mainly because therapeutic compounds cannot cross the blood-brain barrier, a protective membrane that prevents large molecules in the blood from reaching the brain.
A recently developed gene therapy called chimeric hSGSH has shown promising preclinical results in treating mice with MPS III.
It delivers the correct version of the gene that provides instructions to make the heparan N-sulfatase enzyme, but with certain modifications, allowing it to cross the blood-brain barrier.
Previous studies have suggested that the buildup of heparan sulfate can impair the function of enzymes associated with other MPS disorders, leading to secondary tissue accumulation of different GAGs.
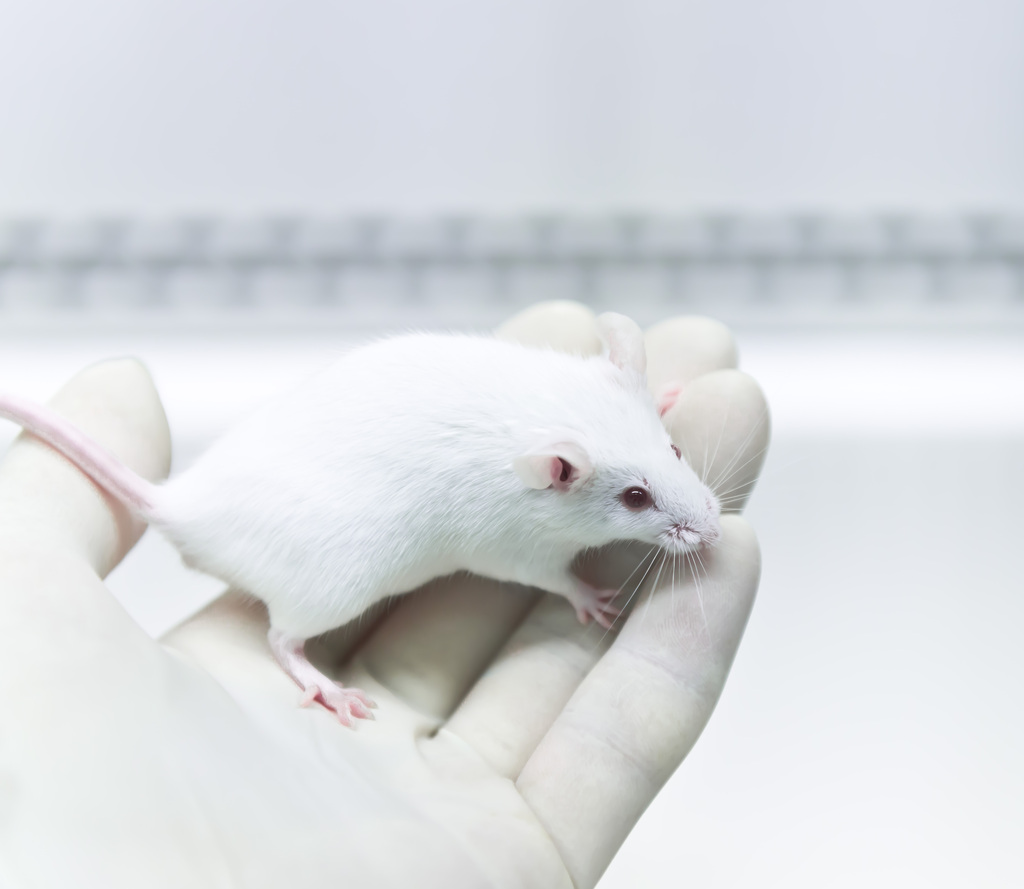
Using an MPS IIIA mouse model, Italian researchers evaluated the accumulation of heparan sulfate and other GAGs — chondroitin sulfate, dermatan sulfate, and hyaluronic acid — in different tissues, as well as the therapeutic effects of chimeric hSGSH treatment.
GAGs were measured in the liver, brain, kidney, and lungs of 8-month-old animals.
Compared to healthy mice, Sanfilippo type A mice had a more severe accumulation of heparan sulfate (15-24 times higher), chondroitin sulfate/dermatan sulfate (two to five times more), and hyaluronic acid (around 2.5 to five times more) in all analyzed organs.
The researchers said this was the first evidence of an association between MPS IIIA and hyaluronic acid — which is known to have a role in inflammation — suggesting the potential involvement of hyaluronic acid in disease worsening and brain damage in MPS IIIA.
“This novel secondary storage discovered in our animal model may have important implications for a full understanding of the molecular mechanism of this disease in particular as a factor responsible for the development of the neuronal pathology,” the researchers wrote.
After the mice received hSGSH gene therapy at 1 month old, the levels of all analyzed GAGs in the brain, liver, and lungs reduced to values similar to those observed in healthy mice, showing the therapy’s potential to effectively treat the disease, specifically the associated brain damage.
However, treatment did not significantly reduce GAG levels in the kidneys. Researchers hypothesized this could be related to the nature of the gene therapy, which targets the liver for the production of the modified enzyme, which in turn mostly targets the brain.
This may reduce the amount of available enzyme to reach other organs.
Researchers believe these data “may have implications for the evaluation of an effective therapeutic option of MPS IIIA and for the reduction of related neuropathology.”