Researchers Develop Stem Cell Line to Study Sanfilippo Syndrome Type B
Written by |
Researchers at the National Institutes of Health have developed an induced pluripotent stem cell (iPSC) line from a 1-year-old child with a mutated NAGLU gene, the gene responsible for Sanfilippo syndrome type B.
These cells may now be used to generate other mature cells, such as neurons, to investigate the mechanisms underlying the disease.
The study, “An induced pluripotent stem cell line (TRNDi006-A) from a MPS IIIB patient carrying homozygous mutation of p.Glu153Lys in NAGLU gene,” was published in Stem Cell Research.
Sanfilippo syndrome type B, also known as mucopolysaccharidosis type IIIB (MPS IIIB), is a rare genetic lysosomal storage disorder caused by mutations in the NAGLU gene, which provides instruction to make the alpha-N-acetylglucosaminidase (NAGLU) enzyme.
NAGLU is responsible for breaking down long complex sugar molecules called heparan sulphate. The reduced activity of NAGLU causes the heparan sulfate to accumulate inside lysosomes — compartments within cells that digest and recycle different types of molecules — resulting in severe neurological impairments. Why this occurs, however, is not completely understood.
Currently there are no effective therapies for Sanfilippo syndrome type B; patients are given therapies to minimize its symptoms.
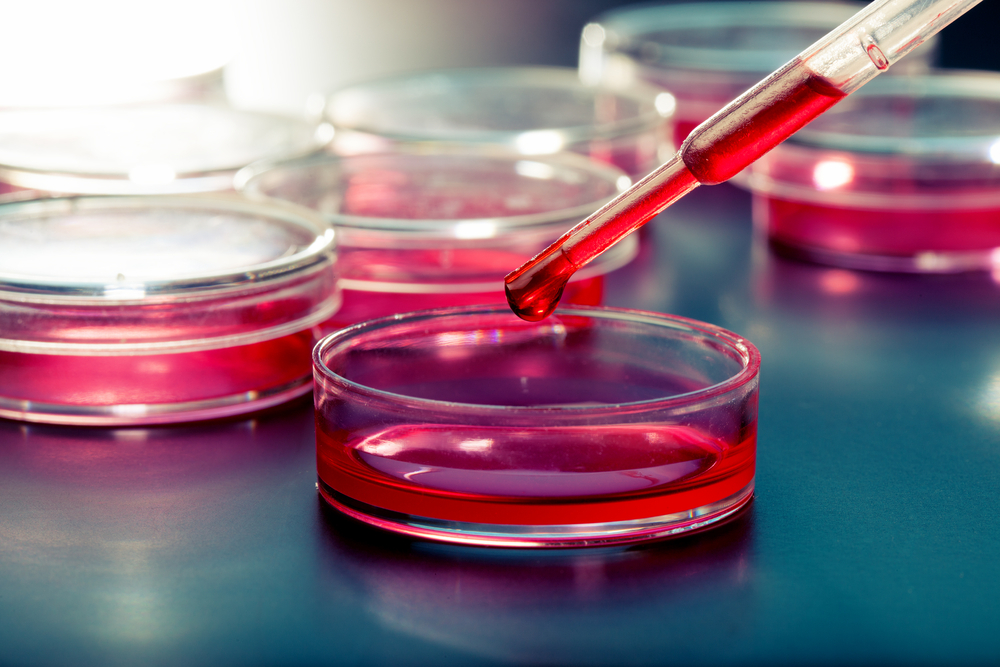
In this study, researchers developed an induced pluripotent stem cell (iPSC) line from skin cells, called fibroblasts, of a 1-year-old with a mutation in both copies of the NAGLU gene.
iPSCs are derived from either skin or blood cells that have been reprogrammed back into a stem cell-like state, which allows for the development of an unlimited source of almost any type of human cell needed for therapeutic purposes.
Researchers called this new cell line TRNDi006-A.
iPSC cells were injected into mice and were able to give rise to the three layers of tissue found in an embryo — ectoderm, mesoderm, and endoderm – from where all other tissues in the body originate.
These results suggest that scientists can now use this cell line to generate mature cells, such as neurons, and study molecular mechanisms underlying this disease. The TRNDi006-A cell line can also be used to test therapies to prevent disease progression.
Overall, “this TRNDi006-A iPSC line is a valuable resource for elucidating the disease phenotype and pathophysiology of MPS IIIB,” researchers said. “It can be differentiated into various mature cell types for use as cell-based disease models of MPS IIIB for compound screening and drug development.”