New Sanfilippo-like Cell Lines Created from Stem Cells, Study Contends
Written by |
Two types of nerve cells, namely neurons and astrocytes, with Sanfilippo syndrome-like characteristics have been created by converting stem cells with disease-associated mutations, according to a study from researchers in Europe.
Compared to cell lines currently used in Sanfilippo research, these new cell lines better mimic disease mechanisms, which should support the development of new therapies.
The study, “Neuronal and Astrocytic Differentiation from Sanfilippo C Syndrome iPSCs for Disease Modeling and Drug Development,” was published in the Journal of Clinical Medicine.
The majority of studies investigating the underlying neurodegenerative disease mechanisms of Sanfilippo syndrome have used non-neural cells such as fibroblasts, the most common cells of connective tissue.
However, fibroblasts and neurons have significant differences that highlight the importance of generating new relevant cell models to understand disease pathology and develop treatments.
Induced pluripotent stem cells (iPSCs) usually are derived from either skin or blood cells and then are reprogrammed back into a stem cell-like state, which allows for the development of an unlimited source of almost any type of human cell needed for therapeutic purposes.
Recently, a team of researchers based at Lund University in Sweden, in collaboration with scientists at the University of Barcelona in Spain, developed three types of iPSCs: one line from a Sanfilippo syndrome type C patient’s fibroblasts, and two cell lines created from cells that carried mutations found in the HGSNAT gene, the genetic cause of Sanfilippo syndrome type C.
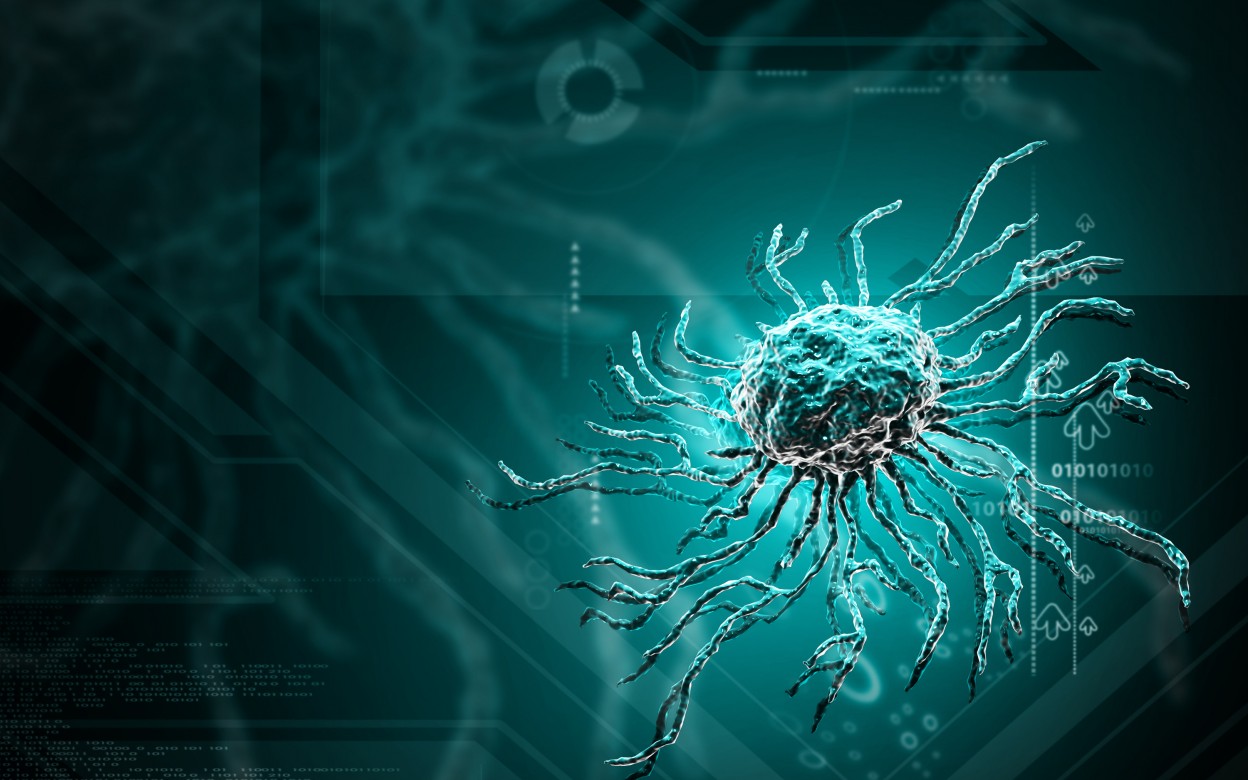
The team converted these cell lines (plus a control cell line) into neurons and astrocytes, which are specialized cells that support neurons, repair nerve cell damage, and help maintain the blood-brain barrier. The validity of each cell line as a Sanfilippo cell-based model system was investigated.
After confirming the conversion to neurons and astrocytes by identifying cell type-specific markers, two different tests were performed to determine if these cells mimicked disease characteristics.
The hallmark of Sanfilippo syndrome is the buildup of glycosaminoglycans, a type of long complex sugar molecules that include heparan sulfate (HS). Accumulation of HS in cellular structures known as lysosomes — the cell compartments responsible for digesting and recycling different types of molecules — causes brain atrophy (shrinkage) and gradual cognitive decline.
The team analyzed changes to the content of lysosomes and measured the levels of heparan sulfate.
While an increase in the area occupied by lysosomes was found in only one of the neuronal cell lines (that harbored HGSNAT mutations), all disease cell lines showed increased levels of lysosomal content compared to a control cell line.
An increase in levels of heparan sulfate also was found in all disease cell lines compared to control cells, which represented the major cellular characteristic of Sanfilippo syndrome.
Researchers then tested an experimental treatment based on blocking the early-stage production of heparan sulfate at the genetic level.
Compared to control cells, in which heparan sulfate levels were reduced, there was no decrease in heparan sulfate levels in neurons derived from one of the disease cell lines (that harbored HGSNAT mutations).
These results contrast with previous results obtained with patient fibroblasts in which heparan sulfate levels were decreased significantly.
“Our data highlights the importance of using appropriate relevant human cell types in future studies to avoid the limitations of using somatic cells to model neurodegenerative diseases,” the researchers wrote.
“We strongly anticipate that [induced neurons] and [induced astrocytes] will be useful tools to rapidly evaluate therapeutic strategies in relevant human brain cell models of neurological disorders,” they added.