Exome Data That Include Unknown Genetic Variants May Better Estimate Sanfilippo Type B Incidence, Study Says
Written by |
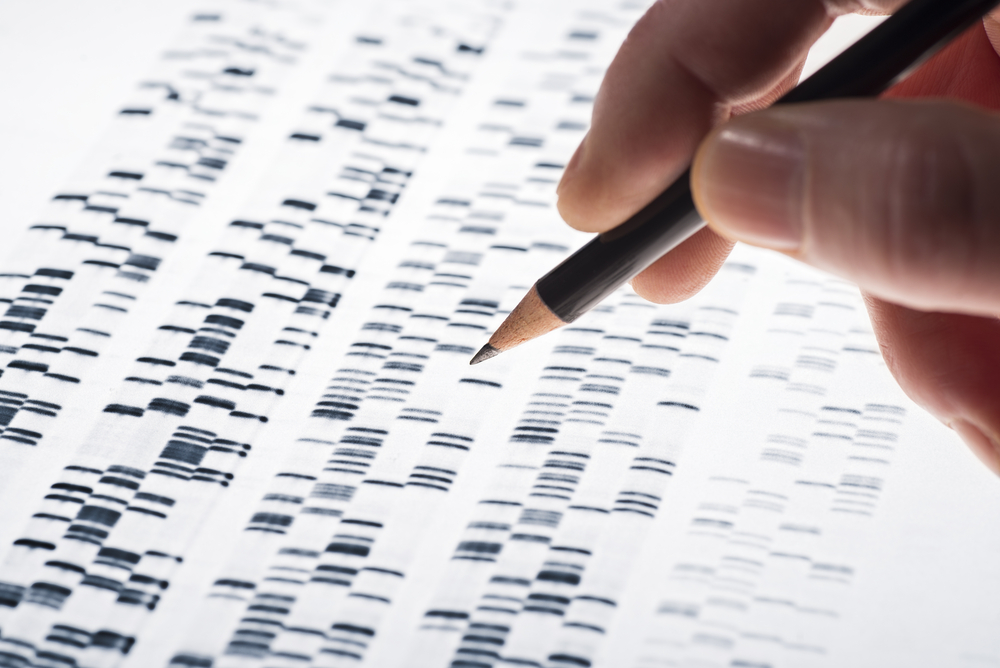
Exome sequencing data — the DNA sequence of all genes encoding for proteins — that include the contribution of variants of unknown significance (VUS), may allow researchers to estimate accurately the incidence of rare genetic disorders, including Sanfilippo syndrome type B, a study suggests.
The study, “Utilizing ExAC to assess the hidden contribution of variants of unknown significance to Sanfilippo Type B incidence,” was published in PLOS One.
Obtaining an accurate estimate of disease incidence for rare genetic disorders is difficult for several reasons, including inaccurate patient registries and limited disease screenings. Alternatively, scientists could attempt to estimate disease incidence of a disorder by calculating the combined rate of mutation carriers in a given population.
“For a population in equilibrium one would simply need to know which variants cause disease, and obtain an estimate of their frequencies in the population of interest. However, large scale sequencing datasets contain an abundance of variants of unknown significance (VUS, or a genetic variant whose biologic impact is unknown),” the investigators said. “Not taking such variants into consideration can potentially lead to the underestimation of disease incidence.”
In the study, a group of researchers tested whether using exome sequencing data to estimate the rate of mutation carriers, taking into account the contribution of VUS, might allow for better estimations of Sanfilippo syndrome type B incidence in Europe.
Sanfilippo syndrome type B, also known as mucopolysaccharidosis type IIIB (MPS IIIB), is a rare genetic lisosomal storage disorder caused by mutations in the NAGLU gene, which provides instruction to make the alpha-N-acetylglucosaminidase (NAGLU) enzyme.
Using the ExAC dataset, an online database containing exome sequencing data from more than 60,000 individuals, the researchers found 189 different missense (single nucleotide mutation that alters protein composition) mutations in the NAGLU gene. From these, 24 had been previously linked to Sanfilippo type B. The remaining 165 were VUS, whose potential contribution to disease was unknown.
The scientists then used cells cultured in a lab to measure the enzymatic activity of NAGLU associated with 164/165 NAGLU missense VUS present in the ExAC dataset, and they developed a statistical approach to estimate the contribution of VUS to the incidence of Sanfilippo type B.
Results showed that 25% of VUS led to a reduction in the activity of NAGLU to levels consistent with other harmful mutations previously linked to Sanfilippo type B.
According to estimations, more than half of Sanfilippo type B cases (67%) were caused by novel genetic mutations that had never been found in patients. This illustrated “the utility of combining functional activity data for VUS with population-wide allele (variant forms of the same gene) frequency data in estimating disease incidence,” the researchers wrote.
“The data in this paper shows that ExAC enables reasonable estimates of disease incidence for rare monogenic (single gene) disorders in the European population, as long as one takes into account the contribution of potentially pathogenic (harmful) VUS. Considering the large number of VUS in ExAC present in other genes, we anticipate this finding will be replicated. Thus, VUS should be considered when performing the same task for other disorders,” they concluded.