Novel Approach Holds Potential to Target Type B Neurological Defects
Written by |
Scientists have discovered a potential novel approach to possibly correct the neurological features of Sanfilippo syndrome type B and other forms of the disease characterized by the accumulation of heparan sulfate and progressive neurodegeneration.
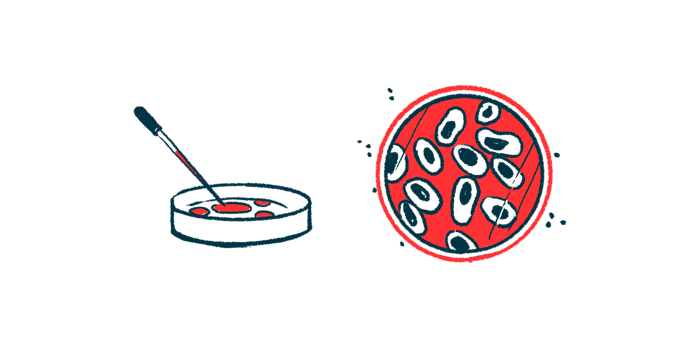
Using a cellular model of Sanfilippo type B, the researchers found that clearing excess levels of heparan sulfate (HS) outside nerve cells reduced lysosomal defects and HS toxic buildup inside cells, restoring their ability to grow and mature.
HS clearance outside cells was obtained through treatment with lab-made NK1, a protein that naturally binds to HS to exert its action.
These findings highlight NK1’s therapeutic potential, as well as of this type of approach, for the treatment of all forms of Sanfilippo syndrome, but more studies are needed to assess whether similar benefits are observed in animal models, the researchers noted.
The study, “Competitive binding of extracellular accumulated heparan sulfate reduces lysosomal storage defects and triggers neuronal differentiation in a model of Mucopolysaccharidosis IIIB,” was published in the journal BBA Molecular Cell Research.
Sanfilippo syndrome, also known as mucopolysaccharidosis type III (MPSIII), is characterized by the toxic accumulation of heparan sulfate, a complex sugar molecule, inside lysosomes due to deficiencies in one of four enzymes that break it down. Lysosomes are cellular compartments responsible for breaking down and recycling molecules.
HS is a component of the extracellular matrix, a three-dimensional and complex network of structural proteins and other molecules that not only supports and surrounds cells of all tissues and organs, but also provides biochemical signals that regulate cell function.
Given that nerve cells, or neurons, are particularly sensitive to HS buildup, Sanfilippo is characterized by progressive and severe neurodegeneration.
Increasing evidence shows that HS accumulates not only inside lysosomes, but also at the cell surface and extracellular matrix in both patients and mouse models of Sanfilippo.
This extracellular buildup has been shown to affect normal signaling and function of cells, including neurons, suggesting an important role for excess levels of HS outside cells in the development of this condition.
Now, a team of researchers at University of Naples Federico II, in Italy, evaluated whether reducing extracellular HS levels could lessen disease features in a neuronal cellular model of Sanfilippo type B (MPSIIIB), which is caused by mutations in the NAGLU gene. The study was funded by the Cure Sanfilippo Foundation.
The cellular model, consisting of lab-grown immature human neurons lacking NAGLU, recapitulated (or mimicked) the disease’s lysosomal defects, as well as heparan sulfate buildup inside and outside cells.
The researchers found that, in contrast to their healthy counterparts, these modified immature cells were unable to mature when stimulated, further supporting the impact of excess HS in neuronal function.
The team used lab-made NK1 as a potential extracellular HS-clearing treatment. NK1 is a natural variant of hepatocyte growth factor (HGF) that strongly binds to extracellular HS to exert its actions, ultimately helping to remove it from around the cells. Both HGF and NK1 are involved in cell growth, development, and communication.
Results showed that treating NAGLU-lacking immature neurons with NK1 reduced HS levels both inside lysosomes and at the cell surface, lessened lysosomal defects, and restored the cells’ ability to mature.
Moreover, NK1 treatment was also able to reduce HS buildup in the resulting mature neurons.
These data “strongly suggest that NK1 treatment, with its action to bind and reduce the HS accumulated in the NAGLU-silenced [immature neurons], is able to reactivate signals necessary for [neuron maturation] and generate undiseased neurons,” the researchers wrote.
As such, these findings highlighting the benefits of HS clearance outside cells “might be relevant for the development of new therapeutic strategies for the cure of MPS IIIB as well as of other MPS types and lysosomal storage diseases characterized by severe neurological [damage],” the team added.
Still, more studies are needed to understand the underlying mechanisms of NK1’s benefits, such as the intracellular signaling pathways it activates, and to confirm its therapeutic potential in animal models.
One of the authors has an Italian patent on compositions comprising HGF or variants thereof for use in the treatment of mucopolysaccharidoses, including Sanfilippo.