Altered Dopamine Signaling May Underlie Autistic-Like Behaviors
Written by |
Altered heparan sulfate metabolism, the underlying cause of Sanfilippo syndrome, leads to dopamine-dependent and autistic-like behaviors in mouse models, a study reported.
Treatment with compounds that blocked dopamine-related pathways rescued hyperactive behaviors and social deficits in these mice, suggesting that dopamine-related therapies may ease the severe autistic-like behaviors seen early in Sanfilippo patients, the scientists said.
The study, “Altered heparan sulfate metabolism during development triggers dopamine-dependent autistic-behaviours in models of lysosomal storage disorders,” was published in the journal Nature Communications and co-funded by Cure Sanfilippo Foundation and the Sanfilippo Children’s Foundation.
Sanfilippo syndrome type A, also referred to as mucopolysaccharidosis IIIA (MPS III), is caused by mutations in the SGSH gene, which encodes for an enzyme that helps break down the complex sugar molecule heparan sulfate. Because of these mutations, heparan sulfate builds to toxic levels inside cells, causing damage, especially in the brain, ultimately leading to neurodegeneration and dementia.
In children with Sanfilippo, dementia is preceded by severe and debilitating autistic-like behaviors, including restlessness and chaotic, anxious, and aggressive actions. These behaviors are so common in Sanfilippo that they often lead to a misdiagnosis of autism spectrum disorder (ASD).
Heparan sulfate and its related proteins form the extracellular matrix that surrounds and supports dopaminergic neurons, or nerve cells in the brain that produce dopamine, a nerve cell signaling molecule involved in body movement, cognition, executive function, reward, and motivation. As a result, heparan sulfate may play a role in regulating dopaminergic neurons.
However, the impact of the heparan sulfate buildup on the regulation of the dopaminergic system and, consequently, on autistic behaviors in Sanfilippo is unknown.
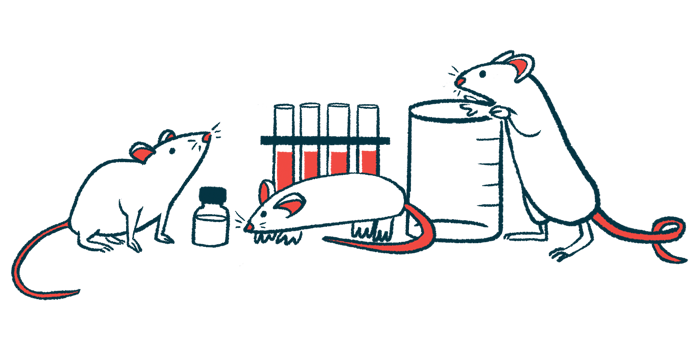
Scientists at the Institute of Biochemistry and Cell Biology, in Italy, used mouse and cell models of Sanfilippo to examine autistic-like features and the disease’s impact on the dopaminergic system.
“Targeting autistic-like symptoms represents an urgent unmet clinical need in [Sanfilippo] patients,” the team wrote. “Some autistic-like behaviors have already been described … however, a full characterization has not been performed.”
Mice (ages 2, 6, and 8 months) with the faulty Sgsh gene initially underwent motor and behavioral assessments using the open field and social interaction tests, such as the social tube test and the three-chamber social preference test.
Two-month-old Sanfilippo A mice were hyperactive in the open field test, as determined by total distance traveled and maximum speed. Social interaction was significantly impaired in these mice, as seen by stereotyped behaviors and consistent social withdrawal when confronted with an unfamiliar healthy mouse. In the social novelty preference task, Sanfilippo A mice lacked a preference for the social stimulus over a new object.
As expected, young Sanfilippo A mice showed no impaired muscle function. In contrast, 8-month-old mice became less active in the open field test but showed no social interaction deficits. Mice at 6 months demonstrated a mixed set of behavioral impairments, suggesting that “the shift from autistic- to dementia-like behaviors was progressive,” the researchers wrote.
To understand the biological mechanisms leading to autistic-like behaviors, the team analyzed the striatum, an area of the forebrain responsible for motor and reward systems that contain dopaminergic neurons. Here, dopamine acts on the protein receptors D1 and D2 on other neurons that are thought to regulate behavior.
Higher expression (production) of the tyrosine hydroxylase (TH) — the enzyme that generates dopamine — was seen in 2-month-old Sanfilippo A mice compared with healthy controls. There was also an increase in the expression of the D1 dopamine receptor, but not the D2 receptor.
“Altogether these findings suggest that [D1 dopamine receptor] direct pathway overactivation might be responsible for some of the behavioral deficits observed in young [Sanfilippo] mice,” the researchers added.
To explore this, mice were injected with alpha-MPT, a molecule that selectively blocks TH. Alpha-MPT did not affect healthy control mice, but it rescued the hyperactive behaviors of Sanfilippo mice in the open field test and social deficits in the social dominance tube test.
A compound that blocked the D1 receptor was tested in a similar experiment. Again, treatment rescued deficits in exploratory activity (distance traveled in the open field test), social interaction in the social tube, and the social novelty test in the Sanfilippo mice.
“These data provide proof-of-concept evidence that preventing TH activation or blocking [D1 receptor] activation rescues hyperactivity and social interaction deficits in [Sanfilippo A mice], indicating a possible disease mechanism and disease-specific therapeutic approaches for autistic-like behavior,” the scientists wrote.
In 2-month-old Sanfilippo A mice, the increase in TH expression was due to a rise in the number of dopaminergic neurons, which was also evident in newborn mice and during the embryonic stage.
“These ex vivo findings report an increased proliferation of dopaminergic cells in [Sanfilippo A mice] embryos as compared to [healthy mice], which is maintained during postnatal life,” the scientists added.
Cell-based experiments showed the increase in dopaminergic neurons was due to the altered function of heparan sulfate. Scientists modified a Sanfilippo A cell line with a functional human SGSH gene, which decreased the number of TH-positive neurons. Then, heparan sulfate treatment reduced cell growth in a dose-dependent manner, “suggesting that the [heparan sulfate] signaling pathway plays a significant role in [TH-postive] cell proliferation,” the researchers noted.
“These in vitro findings show that loss of SGSH gene function leads to altered [heparan sulfate]-function, which contributes to increased [dopaminergic] cell proliferation in [Sanfilippo A],” they added.
Finally, the team wondered if a mouse model of mucopolysaccharidosis II (MPS II), known as Hunter syndrome, also caused by mutations that lead to heparan sulfate buildup, showed autistic-like behaviors and dopamine-related defects.
In the open field test, MPS II mice showed no change in motor activity but greater stereotyped behaviors. Although not generally moving away from others in the social tube test, they avoided other mice in the social interaction test. Notably, the mice also showed increased TH-positive cells and TH expression in the striatum.
“Our findings report a proof-of-concept, pre-clinical evidence on the use of D1R antagonists to treat autistic-like behaviors in [Sanfilippo A],” the researchers concluded.
“Furthermore, the autistic-like behaviors and dementia-like stages can be phenotypically dissociated in terms of behavioral patterns and dopaminergic status, suggesting that parallel disease mechanisms might concurrently lead to autistic-like and dementia-like symptoms in [Sanfilippo A],” they added.