Gene Therapy With More Effective Carrier Shines in Mouse Study
Written by |
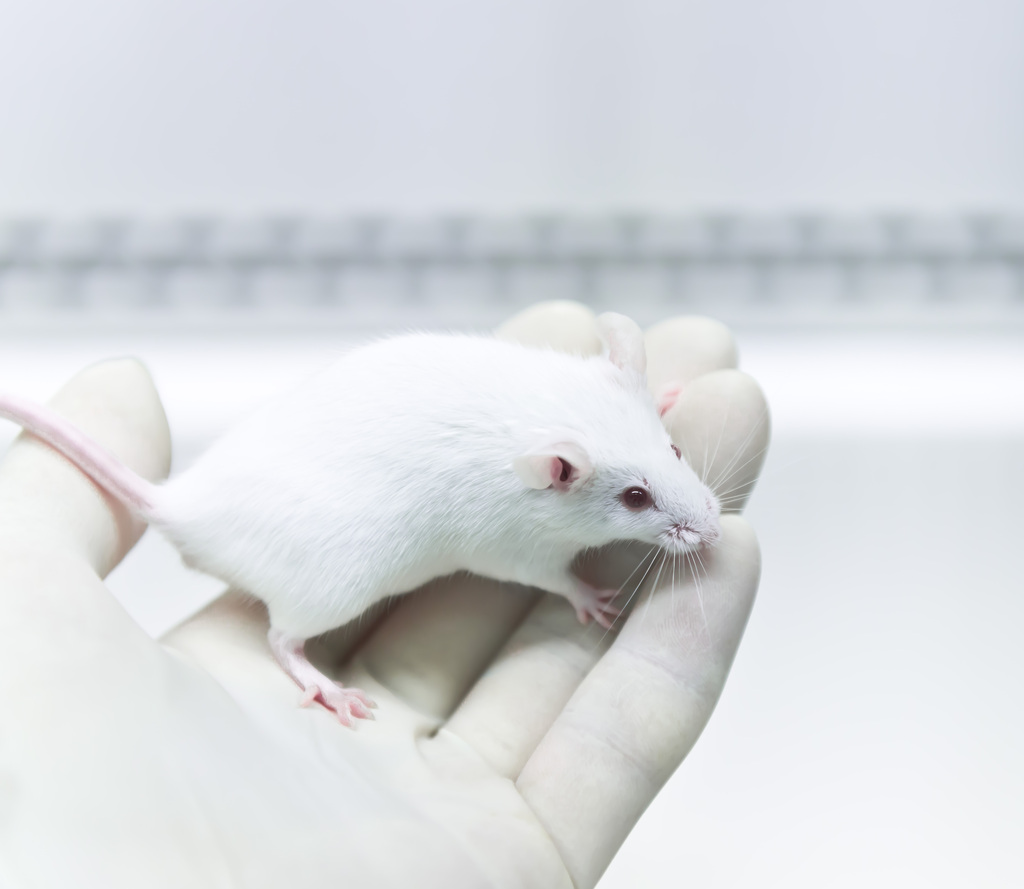
A gene therapy delivered through a more effective viral carrier safely and effectively corrected enzymatic deficiency, restored cognitive and motor function, and improved survival in a mouse model of Sanfilippo syndrome type A, a study shows.
The findings suggest this may be a more effective gene therapy approach to prevent and reverse the broad symptoms of this condition, and support its evaluation in future clinical trials, the researchers noted.
The study, “Targeting the Root Cause of Mucopolysaccharidosis IIIA with a New scAAV9 Gene Replacement Vector,” was published in the journal Molecular Therapy-Methods & Clinical Development.
Sanfilippo syndrome type A, also known as mucopolysaccharidosis type IIIA (MPS IIIA), is caused by mutations in the SGSH gene that result in a deficiency in the enzyme sulfamidase, leading to the toxic accumulation of large sugar molecules, called glycosaminoglycans (GAGs), including heparan sulfate.
While this toxic buildup occurs throughout the body, nerve cells are particularly sensitive to heparan sulfate accumulation. As such, the central nervous system (CNS, the brain and spinal cord) is most affected in these patients, who develop progressive and severe neurodegeneration.
Gene therapy has gained increasing interest for the treatment of Sanfillipo syndrome, as it has the potential to target its underlying cause and delay or prevent neurodegeneration. It works by delivering a functional copy of the mutated gene to cells, ultimately increasing or restoring the levels of the missing protein or enzyme.
Several gene therapies are currently being tested in people with Sanfilippo type A, and some have shown promising, preliminary trial results. Some are administered directly into the bloodstream, while others are injected into the brain. But all use modified and harmless adeno-associated viruses (AAVs) to transport and deliver the gene-of-interest to target cells.
Now, researchers at the University of North Carolina School of Medicine and its Gene Therapy Center developed a potentially improved gene therapy for Sanfilippo syndrome type A that uses a self-complementary AAV type 9 (scAAV9).
Used in clinical-stage and approved gene therapies, AAV9 is known to have the ability to cross the blood-brain barrier, — a protective membrane that prevents certain molecules carried in the blood from entering the brain — thereby allowing CNS targeting.
Its self-complementary version shortens the number of steps required to make the protein-of-interest from the delivered gene, making it a more efficient version.
The newly-developed scAAV9 was designed to deliver a working version of the human SGSH gene to cells in the CNS and peripheral organs, in order to increase sulfamidase activity levels and reduce or prevent GAG and heparan sulfate toxic accumulation.
The team tested the long-term therapeutic effects of three doses — 2.5×1012, 5×1012, and 1×1013 vector genomes (vg)/kg — in a mouse model of the disease at three different ages (1, 3, and 6 months old). The therapy, named scAAV9-hSGSH, was given directly into the bloodstream.
Results showed that a single administration at either dose led to a fast and sustained increase in sulfamidase activity levels in all evaluated tissues of these mice, including peripheral organs and the brain. While these levels differed across tissues (between lower- and higher-than-normal levels), they resulted in a significant drop of GAG contents in all tissues to levels comparable to those seen in healthy mice.
Notably, these benefits were accompanied by a normalization of cognitive and motor functions and improved survival, with most of the mice living normal lifespans.
In addition, no adverse side effects or treatment-related tissue abnormalities were seen in treated mice, suggesting a favorable safety profile.
These findings suggest the gene therapy can “not only prevent but also reverse the disease progression of MPS IIIA in mice,” the researchers wrote, adding that an effective dose can lead to the production of sulfamidase at levels sufficient for GAG clearance throughout the body “regardless of the disease stage to a certain extent.”
The data highlight the “clinically meaningful benefits and the potential of this new [approach] for treating the disease in humans,” they added.
“In summary, we developed a safe and potentially more effective new second-generation scAAV9-hSGSH gene therapy product for the treatment of MPS IIIA,” the researchers wrote.
The study was supported by donations from the Sanfilippo patient community through Aislinn’s Wish Foundation and the Abby Grace Foundation.